Since 2012, more than 85 diseases worldwide have been treated with fecal microbiota transplantation (FMT). The study of the human microbiome has become a continuing trend.
As a branch of discipline within clinical medicine, microbiota medicine holds the potential to significantly influence various aspects of medical education, clinical practice, industry, and the general public. Its far-reaching impact will lead to the emergence of novel discoveries, groundbreaking inventions, and transformative innovations. As a physician and researcher in microbiota medicine, in fact, I never expected or planned to go beyond microbiota technology to establish a discipline. However, during 11 years of various conflicts, I have been reflecting on the fundamental aspects and future of microbiota technology in clinical medicine. This reflection has led me to think beyond the value and dimensions of technology, proposing the establishment of microbiota medicine as a discipline. My co-authors and I recently discussed the concept, dimensions, and development of microbiota medicine in Microbial Biotechnology. I am delighted to have been invited by Dr. Matthew Koch to share my insights on microbiota medicine with the readers of The Microbiologist.
Patients benefit from microbiota technology
Curiosity drives researchers to explore the microbiota technology in medicine. In 2013, the scientific community predicted that the study of the microbiome would bring revolutionary breakthroughs in the diagnosis and treatment of inflammation and immune-related diseases.
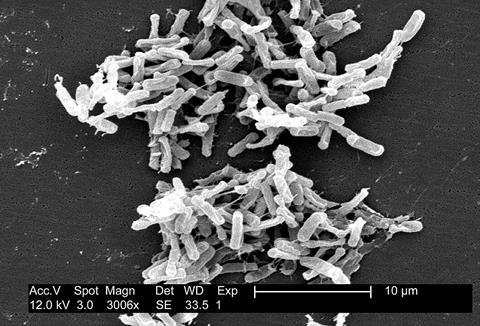
Fecal microbiota transplantation (FMT) has proven in an extreme manner that the human gut microbiota plays a significant role in the occurrence of various diseases. A systematic study published in the Chinese Medical Journal in 2022 on global FMT clinical reports revealed that since the term “fecal microbiota transplantation” was formally defined in 2011, it has been used to treat 85 diseases in the past decade. These diseases span across areas such as the digestive system, immune system, nervous system, and urinary system.
“As early as a decade ago, there were commercial capital investments in the United States that used faecal matter from healthy donors for disease treatment, and even promoted the faeces of celebrities.”
These commercially driven illegal medical practices led to uncontrolled biological safety risks and were quickly banned by the US government. However, this resulted in many patients being unable to access this life-saving treatment and losing their lives. As a result, many doctors called for a relaxation of regulations. Eventually, many governments allowed a small loophole: allowing doctors to use FMT for the treatment of recurrent Clostridioides difficile infections within hospitals. Commercial capital once touted the use of faecal microbiota sequencing to diagnose diseases and find the culprits responsible for changing human health destinies. However, these technology-related utilitarian behaviors, especially the fabrication of various beautiful lies, created huge bubbles that eventually burst.
Today, when we reconsider the history of microbiota technologies in the field of health, we can draw two clear conclusions.
1. FMT can indeed treat Clostridioides difficile infections and other diseases associated with microbiota dysbiosis, but the number of patients worldwide truly benefiting from this technology is still limited.
2. While commercial capital drives industry development, those excessively profit-seeking behaviors ultimately harm the development of clinical medicine.
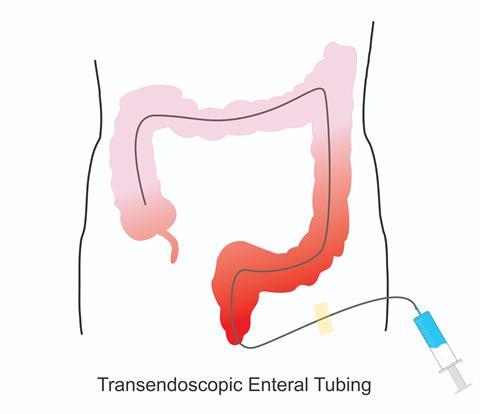
As a medical technology, FMT does not belong to the negative list of technologies regulated by the National Health Commission of China and can be implemented by licensed physicians in hospitals. The technology has gained favourable development opportunities as a non-profit technology service in numerous hospitals in China. We have developed washed microbiota transplantation, using automatic machines instead of humans to handle faeces. We further have discovered that the safety of the washing process is significantly improved when compared to manual faecal microbiota transplantation. In addition, we have invented an endoscopic intervention technique, called transendoscopic enteral tubing, for implanting microbiota into the deep colon. This soft tube is similar to the widely used indwelling intravenous needle, allowing nurses to repeatedly use the infusion tube inside the vein without having to repeatedly puncture the patient.
My team provides washed microbiota transplantation treatment to hospitalised patients at the Second Affiliated Hospital of Nanjing Medical University (Nanjing, China) and offers non-profit remote rescue to patients with intractable intestinal infections nationwide. Currently, we provide washed microbiota transplantation to approximately 200 patients per month. As a national referral centre for microbiota transplantation, the diseases we treat include Clostridioides difficile infections, inflammatory bowel disease, radiation colitis, immune checkpoint inhibitor-associated colitis, diarrhoea following hematopoietic stem cell transplantation, diabetic neuropathy, allergic rhinitis, and childhood autism. Many doctors from various hospitals come to study and learn these new techniques. Some people have raised doubts about this. However, I believe that this is a normal and reasonable skepticism because it challenges the mainstream understanding of medicine, and those in the mainstream naturally strive to restore the old medical order.
Common reasons cited by skeptics include unclear mechanisms, ethical violations, and going beyond medical norms. However, these do not touch upon the core issue: do patients benefit? This is the most fundamental question in clinical medicine and the problem that doctors seek to address in their pursuit of true medical excellence.
The “grave diggers” of traditional medicine disciplines
The diseases that benefit from FMT span across various traditional disciplines, often appearing unrelated. However, these diseases are now categorised under a new family called “dysbiosis-related diseases”.
We initially established the department of microbiota medicine at Nanjing Medical University in Nanjing, China. As a branch of clinical medicine, the department focuses primarily on the use of microbiota transplantation to treat refractory and critically ill “dysbiosis-related diseases”. Our disciplinary team requires comprehensive diagnostic and therapeutic capabilities in diseases related to the digestive system, diabetes, cancers, immune system, kidney diseases, neurological and psychiatric systems, and others. Additionally, we train specialised physicians in hospitals. We offer courses at university level, recruit graduate students, and have already started writing textbooks on microbiota medicine. This is a crucial aspect that differentiates our discipline from clinical technical service divisions. Our original speciality training background was gastroenterology, and now we are venturing beyond the realm of gastroenterology to treat patients who were originally attributed to other disciplines. Such explorers are called the “grave diggers” of traditional medicine disciplines.

Clinical medicine, originally emphasising holistic care, has undergone continuous subdivision in the present day. Professor Fan Daiming, a renowned medical scientist and educator, proposed the concept of holistic integrative medicine and has been dedicated to reuniting fragmented clinical medicine. He has organised numerous medical conferences, authored a series of books, developed guidelines, served as the chief editor of various journals, engaged in dialogue with the government and the public, and established a national research institution for integrated medicine. His efforts have brought significant inspiration and conceptual updates to his peers. “The whole is greater than the sum of its parts,” as Aristotle said. Microbiota medicine is a significant manifestation of holistic integrative medicine, integrating various scattered branches of disciplines.
The “grave diggers” inevitably face contradictions and controversies. The traditional disciplinary framework does not support the “grave diggers” in treating diseases across multiple fields. In order to help the general public, as well as medical professionals, better understand the vital role of the microbiota in human health and disease, and make the invisible microbiome visible, we have established a “Human Microbiota Sect Saloon” with the support of the hospital. It employs immersive projection, pictures, and laboratory windows for visitors to explore the milestones of the human microbiota throughout history.

Microbiome technology extends beyond FMT, and the development of this field in medicine has reached a bottleneck. Now is the time to discuss key questions:
“Where is this field heading? How can we achieve sustainable development goals?”
Although many scientific questions remain unanswered, scientists and doctors have built many stepping stones and have the conditions to advance new explorations. The technology of washed microbiota transplantation has made the procedure safer. Alcohol-based spore enrichment has become a pharmaceutical technology, and colonic transendoscopic enteral tubing enables repeated transplantation and real-time dynamic sampling of the entire colon for the study of microbiota-host interactions. Deep sequencing-based big data mining techniques have provided new research tools for understanding the complex functions of the microbiome.
Microbiota medicine nurtures inventions, discoveries, and even great innovations
The development of microbiota medicine worldwide requires a large number of “grave diggers”. In China, not only in Nanjing but in many cities across the country, dozens of hospitals are developing microbiota medicine technologies. For example, Professor He Xingxiang in Guangzhou and Professor Yuan Huijuan in Zhengzhou have distinctive teams. To resolve the conflicts faced by the “grave diggers”, microbiota medicine needs to be incorporated into the framework of clinical medicine, changing the patterns of clinical practice and disease prevention. This new concept will directly impact the content of clinical medicine education, the framework of clinical practice, the mode of medical research, and microbiome pharmaceutical technology.
Microbiota medicine is becoming a new discipline of clinical medicine, meeting the following conditions:
1. It has a specific conceptual system that supports the formation and development of microbiota medicine concepts, such as metagenomics, which has been widely used in medical research.
2. A network of relationships among these concepts has formed to serve clinical needs in the prevention, diagnosis, and treatment based on microbiome research, establishing specific logical structures such as the gut-brain axis.
3. Knowledge based on the microbiome can be validated through clinical experience, such as health issues in the post-antibiotic era.
4. Specific techniques have been developed to promote the development of microbiota medicine, such as microbiota transplantation and innovative approaches for timely transplantation.
Microbiota medicine should not be confused with medical microecology (or medical microbiology), just as anatomy and surgery have essential differences in their tasks. Medical microecology belongs to the realm of basic medicine, with the core task of rational medicine. Microbiota medicine belongs to the realm of clinical medicine, with the core task of effective diagnosis and treatment.
Microbiota medicine needs to gradually establish its own “ecological niche” in medicine, cultivate medical talents in the long term, and continuously promote the technical system of the discipline. The development of the discipline of microbiota medicine is very interesting, as it resembles the dynamic evolution process of the microbiome itself – invisible to the naked eye and initially difficult for people to understand. However, it has outstanding characteristics of openness, borderlessness, slow development, and powerful generative strength.
The medical talents nurtured in microbiota medicine need to break free from conventional thinking, possess sufficient imagination, and have a holistic perspective. The discipline of microbiota medicine requires a large number of pioneers who believe that opportunities for innovation are fair, and that true innovation cannot be planned but can succeed in any hospital.
The development trajectory of microbiota medicine can be compared to that of transfusion medicine. Analogous to microbiota medicine and transfusion medicine, the substances used for blood transfusion and FMT, respectively, originate from two healthy channels in the human body: the gastrointestinal tract and the blood vessels. The medical technologies derived from both belong to the focuses of all countries’ attention to human health and well-being. Therefore, the development of microbiota medicine as a clinical discipline will affect medicine education, clinical practice, industry, and the general public. We call on teaching hospitals in universities to establish microbiota medicine as a branch of discipline within clinical medicine as soon as possible. Microbiota medicine will create fertile ground to nurture new inventions, discoveries, and even great innovations.








No comments yet